Understanding OCD: A Journey from Diagnosis to Hope (Final Post)
Welcome to the final post of these series. I sincerely hope you have learned something new that can help you in your OCD journey from my posts. Together, we have covered a lot of OCD related aspects, from its definition and preventative measures to therapeutic options and alternative treatments. This post brings the previous discussions together by touching on the link between OCD and quality of life, providing a treatment roadmap for OCD, which you can consult at any point, and a few final words to wrap the series.
Quality of Life
Quality of life (QOL) refers to someone's subjective perception of their well-being. This perception is impacted by the individual's psychological status, physical health, social relationships, the role they play in society (e.g., work) and a sense of life satisfaction.
It is not surprising that OCD significantly reduces QOL in multiple areas, such as family, work, and social life. Additionally, caregivers of individuals with OCD also experience lower QOL when compared to those with healthy children.
QOL in OCD has been inconsistently found to be associated with age, gender, marital status, employment status, socioeconomic status, education level, and lack of social support networks. On the other hand, the severity of OCD symptoms, presence of comorbid depression, and specific symptom dimensions (e.g., hoarding) have been found to be more reliably associated with a decreased QOL and overall functional impairment. Indeed, one needs to pay attention to existing depressive symptoms as they mediate the relationship between OCD and impaired QOL. This underlines the importance of tackling both depression and OCD and not just one or the other.
There does exist an association of psychotherapy and pharmacotherapy with improved QOL in individuals with OCD. Treatment respondents and patients who did not relapse show more promising results in increasing QOL with therapeutic aids, which gives strength to the link between symptom reduction and QOL. Hence, when a patient undergoes therapeutic treatment, the therapist should not only pay attention to treatment response, but also with how a given response is impacting the patient's quality of life. Although good treatment response does not necessarily equate to symptom remission (reduction or elimination of symptoms for a period of time), it can still have substantial improvements in the patient's quality of life.
When it comes to quality of life, people with OCD can be just as impaired as those living with schizophrenia. This comparison matters because the level of functional impairment associated with schizophrenia, while not identical, is more widely recognized by the public. Highlighting this similarity helps put into perspective the very real suffering that can come with obsessive–compulsive disorder. This is not about comparing who suffers more or turning distress into a competition. Different conditions bring different struggles, and all of them deserve to be taken seriously.
OCD Treatment Roadmap
Disclaimer: This roadmap represents a synthesized overview of commonly recommended, evidence-based treatment pathways for OCD and is intended for educational purposes only. It does not replace individualized clinical assessment, guideline-based decision-making, or professional medical advice.
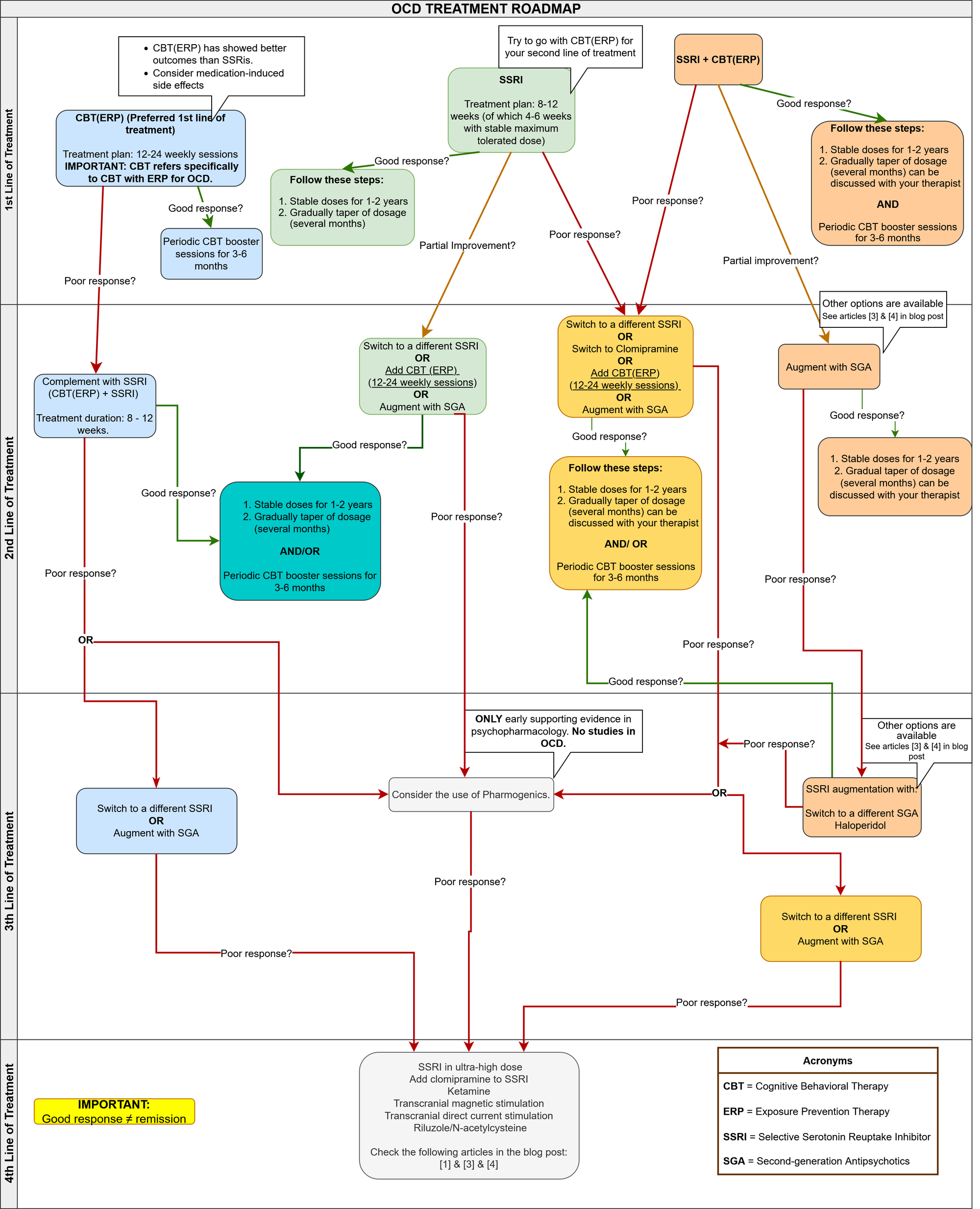
There are a couple of aspects to mention regarding this roadmap. I created it by using the following articles ([1] [3] [4]) while trying to find patterns between the research paper's roadmaps and combine it into one. This, hopefully, ensures that you will get a broader picture of the current evidence-based treatment for OCD.
You may notice that at times I add dialogue boxes stating "Other options are available". These options are, for the most part, treatment options that have (1) too little evidence, (2) lower quality studies, or (3) early evidence exists in psychopharmacology, but not in OCD directly.
Final words
If there is one message I hope you can take from this series, it is that OCD is not a static condition and that there are concrete steps that can be taken to improve quality of life. Progress will most likely not be linear, but gradual with ups and downs. However, scientific evidence consistently shows that meaningful positive change is possible with appropriate support and sustained treatment.
Although I try to make these posts accessible to the general population, there is still a lot of information in them, which can be overwhelming and lower the possibility of you starting your own treatment. It is perfectly reasonable and prudent to simplify. You do not need to understand every concept or mechanism, or even explore every treatment option at once. In practical terms, focusing on the treatment roadmap alone can be enough to get started as it offers a structured overview of evidence-based options, which you can use as a compass. Sometimes all someone needs is direction.
It is also important to remember that improvement is not limited to symptom reduction along. Addressing comorbid difficulties such as depression, poor daily functioning, and restoring one's sense of autonomy are equally important outcomes. These changes often unfold alongside, rather than after, symptom improvement. Please do keep this in mind when measuring overall mental health improvement.
Finally, as you are probably aware, recovery does not mean the absence of difficulty. It means developing the tools, support, and flexibility needed to live a fuller life despite uncertainty. If this series has helped you better understand your options, ask more informed questions, or take even one step forward, then it has served its purpose.
Thank you for taking the time to read my post,
João Carvalho
Article recommendations:
Psychopharmacological Treatment of Obsessive-Compulsive Disorder (OCD)
Treatment of obsessive-compulsive disorders (OCD) and obsessive-compulsive-related disorders (OCRD)
The two articles above were the main inspiration for the roadmap created here. They also provide their own treatment roadmaps. I recommend you check them out for a more complete picture of available treatments.
This is a great initiative with the goal of improving how OCD is conceptualized, diagnosed, and treated worldwide
Sources
[1] D. J. Stein et al., “Obsessive–compulsive disorder,” Nat Rev Dis Primers, vol. 5, no. 1, p. 52, Aug. 2019, doi: 10.1038/s41572-019-0102-3.
[2] A. Singh, V. P. Anjankar, and B. Sapkale, “Obsessive-Compulsive Disorder (OCD): A Comprehensive Review of Diagnosis, Comorbidities, and Treatment Approaches,” Cureus, Nov. 2023, doi: 10.7759/cureus.48960.
[3] Del Casale, A., Sorice, S., Padovano, A., Simmaco, M., Ferracuti, S., Lamis, D. A., Rapinesi, C., Sani, G., Girardi, P., Kotzalidis, G. D., & Pompili, M. (2019). Psychopharmacological Treatment of Obsessive-Compulsive Disorder (OCD). Current Neuropharmacology, 17(8), 710–736. https://doi.org/10.2174/1570159X16666180813155017
[4] Krzyszkowiak, W., Kuleta-Krzyszkowiak, M., & Krzanowska, E. (2019). Treatment of obsessive-compulsive disorders (OCD) and obsessive-compulsive-related disorders (OCRD). Psychiatria Polska, 53(4), 825–843. https://doi.org/10.12740/PP/105130
Disclaimer: Everything I share here comes from my own personal research. This blog is never meant to serve as a substitute for professional advice—if you're struggling, I truly encourage you to reach out to a qualified mental health professional.