Understanding OCD: A Journey from Diagnosis to Hope (Part 1 of 3 in a New Series)
What does it really mean to have OCD and how can you tell if it applies to you? In this first post of a science-based series, we explore how OCD is diagnosed, its prevention, and my thoughts on self-diagnoses. Whether you're navigating a diagnosis or seeking clarity, this guide if for you.
This new series of posts is going to serve as a science-based guide on steps to take and things to keep in mind throughout your OCD treatment journey. This first post will cover the diagnosis and screening process, as well as preventative measures one can take to prevent the manifestation of OCD.
What Is OCD? A Brief Overview
Before delving into the diagnosis, assessment, and prevention of OCD, it's important to gain some foundational knowledge regarding the disorder.
Obsessive-compulsive disorder (OCD) is part of a broader category of disorders known as obsessive-compulsive and related disorders (OCRDs), which may cause severe negative daily functional impairment*.
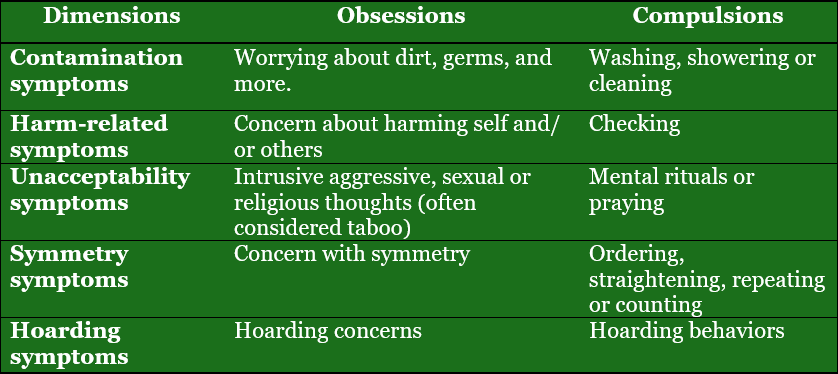
OCD involves the existence of obsessions and/or compulsions (see Fig. 1).
- Obsessions are repetitive and intrusive thoughts, mental images, and urges, which are unwanted and strongly linked to anxiety.
- Compulsions refer to when an individual feels compelled to act out repetitive behaviors or mental acts, usually in response to an obsession. These are often based on rigid rules or are aimed at reducing anxiety or achieving a sense of completeness.
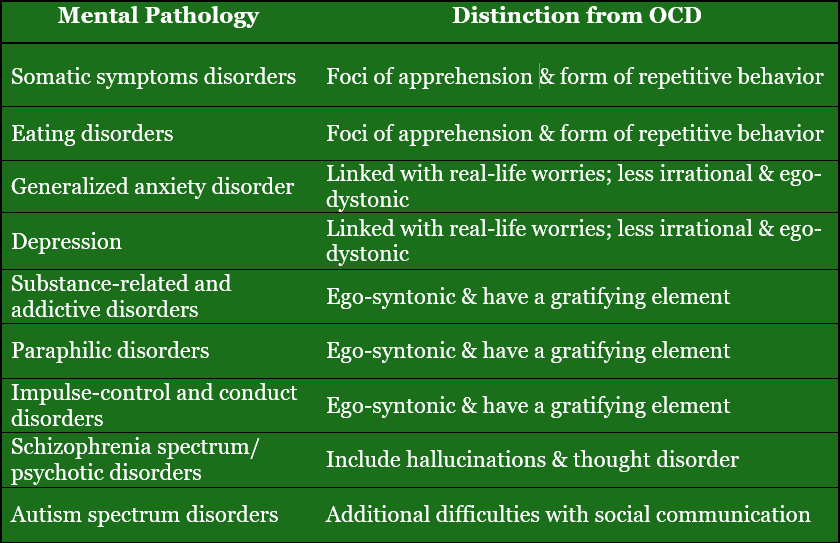
OCD symptoms are typically ego-dystonic, meaning the person recognizes the thoughts or behaviors as unwanted, intrusive, or inconsistent with their values and self-concept. This is part of what causes so much distress.
In contrast, ego-syntonic symptoms are those that feel aligned with a person's beliefs or identity. The symptoms don’t feel “wrong” to the individual. This distinction is crucial in differentiating OCD from other disorders like some personality disorders, where problematic behaviors might be seen as appropriate or justified by the person.
* Functional impairment
The extent a condition interferes with your ability to carry out daily tasks like work, school, relationships, or self-care.
How OCD Affects the Brain and Behavior
OCD Mechanisms
Executive functions* affected by OCD :
- cognitive flexibility
- planning
- working memory
- response inhibition†
Other processes impacted by OCD :
- disgust processing
- fear extinction
- reward processing
- emotion regulation ‡
*Mental processes or skills we use to set and reach goals.
† The ability to stop yourself from doing something automatic or impulsive. People with OCD may find it harder to resist compulsions, even if they know they’re irrational.
‡ The ability to manage and respond to emotional experiences in a healthy way. OCD can make this process harder, especially when emotions like fear or disgust are triggered by obsessions.
Are You at Risk? Genetic and Environmental Factors
Both genetic and environmental factors contribute to the development of OCD.
- Genetics account for approximately 40% of the variance (e.g., family history of OCD).
- Environment contributes about 51% (e.g., birth complications, trauma).
- Gene-environment interactions also play a role. For example, individuals may have a genetic predisposition to experience negative emotions more intensely.
Understanding OCD Diagnosis
Although the diagnosis and screening of mental disorders should be left to health professionals, OCD is often misdiagnosed, mistreated, or entirely missed during routine check-ups. Hence, the general public would benefit from gaining knowledge about how OCD is diagnosed.
DSM-5 Diagnostic Criteria
According to the DSM-5, a diagnosis of OCD involves:
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is a diagnostic tool used by mental health professionals throughout the world.
- Obsessions and/or compulsions that cause clinical levels of distress or functional impairment. Merely having intrusive thoughts or repetitive behaviors does not qualify unless they reach this clinical threshold.
- Symptoms must not be attributable to the effects of a substance or another medical condition.
- Symptoms typically remain within a consistent symptom dimension, though they may evolve within that dimension.
Insight and Tic Specifiers
- Insight Specifiers: The individual’s degree of insight into their OCD beliefs (how much one can distinguish OCD-induced thoughts from their own thoughts) may vary:
- Good or fair insight
- Poor insight
- Absent insight or delusional beliefs (which may lead to misdiagnosis and inadequate treatment). Individuals with this level of insight truly believe their OCD-induced thoughts.
- Tic Specifier: Some individuals also experience tics. Recognizing this is important because OCD with tics may have distinct biological and treatment implications.
Differentiating OCD from Common Behavior
Many people have occasional intrusive thoughts or check things more than once (e.g., checking the oven). To distinguish OCD from typical behavior:
- OCD thoughts and behaviors are time-consuming (usually >1 hour/day).
- They cause distress or impair daily functioning.
Distinguishing OCD from Other Mental Disorders
OCD shares symptoms with various other mental disorders. Proper diagnosis requires differentiating between them:
Screening and Assessment Tools
One of the most important steps in the diagnosis and management of OCD is a thorough mental health assessment. This involves:
- Making an accurate diagnosis
- Gathering detailed symptom information
- Measuring symptom severity
- Identifying symptom targets
- Collecting psychiatric history and mental status
There are a number of assessment measures that have proven efficient in diagnosing OCD.
Diagnostic tools (click on me)
Clinical Diagnostic Interview
- Structured Clinical Interview for DSM-5 for adults
- Anxiety Disorders interview schedule for DSM-5 (adult and child or parent version)
- Mini International Neuropsychiatric Interview
- Structured Clinical Interview for OCRDs (check for comorbidities)
Comorbidity refers to the presence of one or more additional mental health conditions occurring alongside OCD (e.g., depression, anxiety disorders, tic disorders).
OCD Symptom and Severity Scales
- Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) /Children’s Y-BOC (CY-BOCS) - Includes a symptom checklist and severity scale (self-report format)
- The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS) - A more nuanced assessment of both symptom dimensions and severity
- Florida Obsessive-Compulsive Inventory (FOCI) - A shorter tool for symptom checklist and severity, also applicable to other OCRDs.
Additional Tools
- Scales for sensory phenomena
- Insight measures
- Family accommodation (definition in next section) measures
Can OCD Be Prevented?
Unfortunately, there is limited research on the prevention of OCD. However, some preliminary strategies include:
Primary Prevention
- Psychoeducation for families and at-risk individuals*
- Avoiding family accommodation† of compulsive behaviors in those showing early signs
Secondary Prevention
- Early identification and management of subclinical or clinical OCD
- Professional monitoring in those with a family history or risk factors
* At-risk individuals
People that have subclinical levels of OCD or have a pre-disposition for OCD, even if they don't currently exhibit any symptoms.
† Family accommodation
Ways the ones closest to you might unintentionally support or reinforce OCD behaviors (e.g., participating in rituals, offering repeated reassurance), which can worsen symptoms over time.
Final Thoughts
While seeking professional help is the most reliable and safest way to get an accurate diagnosis and proper management for OCD, not everyone has the means or access to mental health services. Even when support is available, it may come slow, which is deeply frustrating when you're suffering and needed help yesterday. So, what can you do in the meantime?
I understand the concerns surrounding self-diagnosis, and I agree that it's not a substitute for professional evaluation. However, dismissing someone's self-assessment outright can invalidate their suffering. These dismissals may come from a just place, especially if an individual is using the self-diagnosed mental disorder as a crutch to diminish accountability. However, a self-diagnosis may come from a place of desperation, which I can completely relate to and empathize with.
Sometimes, individuals suffering from an undiagnosed mental disorder can be placed in a situation, in which help is far away with the only resource left being themselves or the ones close to them. When this is the case, while one still should be held accountable for their actions, possible dismissals of someone's self-assessment by others may come from a place of self-perceived moral superiority rather than empathy or genuine concern.
Do I think self-diagnosis is 100% accurate? Of course not. But do I believe it can have value? Absolutely, though it comes with important caveats. From what I understand about the diagnostic process, the most difficult aspect, even for trained professionals, is differential diagnosis. It's one thing to recognize a set of symptoms, but it's another to determine whether those symptoms point to OCD, another condition, or a combination of both. It can be an incredibly complex task, which even mental practitioners can and do fail at.
Self-diagnosis shouldn't be treated as a definitive conclusion. Rather, it can be a starting point, an opportunity to reflect on your experience, gather information, and momentarily decide what is the best course of action to take in terms of treatment. Needles to say that misdiagnosing yourself isn’t good, but it’s often less damaging than a misdiagnosis from a clinician, which can carry long-term consequences if left uncorrected. Nevertheless, whether or not you have professional help readily available, informing yourself about a disorder you suspect you may have is a good step toward gaining deeper insight into yourself.
OCD is a complex and often misunderstood disorder. Early recognition, accurate diagnosis, and timely intervention are crucial for effective treatment. Although research into prevention is still in its early stages, raising awareness and educating oneself (and others) can make a meaningful difference, especially for those who may be at risk.
In the next post, we’ll explore the different evidence-based treatments for OCD, including Cognitive Behavioral Therapy (CBT), Exposure and Response Prevention (ERP), and pharmacological options.
Thank you for taking the time to read my post,
João Carvalho
Article Recommendation
This is a great initiative with the goal of improving how OCD is conceptualized, diagnosed, and treated worldwide.
Sources
[1] D. J. Stein et al., “Obsessive–compulsive disorder,” Nat Rev Dis Primers, vol. 5, no. 1, p. 52, Aug. 2019, doi: 10.1038/s41572-019-0102-3.
[2] A. Singh, V. P. Anjankar, and B. Sapkale, “Obsessive-Compulsive Disorder (OCD): A Comprehensive Review of Diagnosis, Comorbidities, and Treatment Approaches,” Cureus, Nov. 2023, doi: 10.7759/cureus.48960.
Disclaimer: Everything I share here comes from my own personal research. This blog is never meant to serve as a substitute for professional advice—if you're struggling, I truly encourage you to reach out to a qualified mental health professional.